Can Pupillometry help to detect Delayed Cerebral Ischemia in SAH?
Published:
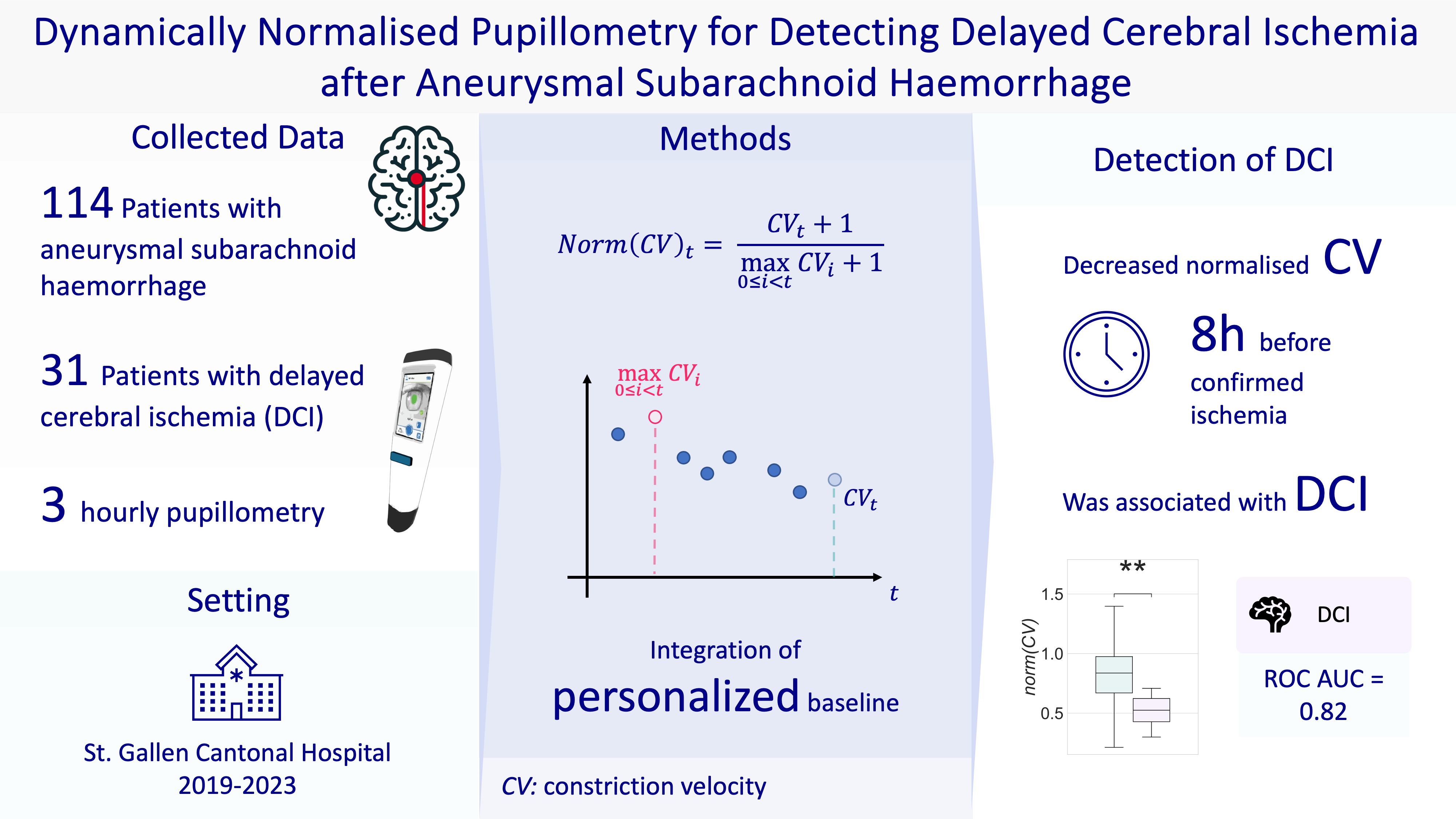
Key Question: Can pupillometry be used to monitor and detect delayed cerebral ischemia (DCI) in patients with aneurysmal subarachnoid hemorrhage (aSAH)?

Context In patients with reduced state of consciousness or non-motor manifestations of ischemia such as confusion, the diagnosis of DCI is often complicated and the currently available tools are limited.
Study Findings In this retrospective cohort study involving 114 patients with aSAH, we found that pupil constriction velocity (CV) normalized to each patient’s maximum recorded value since admission (referred to as normalized CV) was predictive of DCI within 8 hours. The predictive power was strong, with an area under the receiver operating characteristic curve (AUC) of 0.82. Other metrics, such as the Neurological Pupil Index (NPi) and non-normalized measures, were not significantly associated with DCI. Study Details The study was conducted at the ICU of Cantonal Hospital St. Gallen in Switzerland, including all adult patients with aSAH admitted between March 2019 and December 2023. Pupillometry data was collected frequently (every 3 hours on average), allowing for continuous monitoring and normalization to each patient’s best recorded values. DCI was confirmed on perfusion CT.
Features
- CV (constriction velocity): change in pupil size from baseline to minimum over time in response to a light-stimulus
- NPi (Neurological Pupil Index): proprietary scalar index ranging from 0 to 5, with greater than or equal to 3 being a normal value
- Raw and normalized were evaluated
Why Normalize?
- Individual Baseline Differences: Normalization accounts for individual differences in baseline pupillary responses. Each patient has a unique baseline pupillary response, influenced by various factors such as the underlying neurological status, and side of initial injury. Normalizing allows comparisons to be made relative to each patient’s own optimal response rather than using a one-size-fits-all threshold.
- Dynamic Changes Over Time: Normalization helps in capturing the dynamic changes in pupillary function over time. In aSAH patients, the neurological state can fluctuate, and a normalized metric can sensitively reflect these changes. This is particularly important for conditions like DCI, which develop over time and may present subtly at first.
Results
- Predictive Value of Normalized CV: Normalized CV (inter-eye minimum, maximum in an 8-hour timebin) had an AUC of 0.82, indicating good discriminative ability. This metric was found to be the best predictor of DCI within an 8-hour window.
- Non-significance of NPi: The study confirmed that NPi and other non-normalized metrics were not significantly associated with DCI, supporting findings from previous research.
- Long-term Outcomes: Only CV, not NPi, was associated with long-term functional outcomes (measured by the modified Rankin Scale) at one year after adjusting for other factors.
Implications for Clinical Practice Normalized CV offers a new ancillary method for early detection of DCI in aSAH patients. This metric’s high sensitivity makes it a useful tool in the multimodal monitoring of patients, especially those who are sedated or cannot be clinically assessed.
Conclusion Frequent, longitudinal quantitative pupillometry, specifically normalized CV, can effectively predict DCI in aSAH patients. This method provides a personalized monitoring approach that could improve early detection and management of DCI, potentially enhancing patient outcomes.
Full paper: Klug, Julian; Martins, Joana; De Trizio, Ignazio; Carrera, Emmanuel; Filipovic, Miodrag; Hostettler, Isabel Charlotte; Pietsch, Urs. Dynamically Normalized Pupillometry for Detecting Delayed Cerebral Ischemia After Aneurysmal Subarachnoid Hemorrhage. Critical Care Explorations 6(8):p e1135, August 2024. | DOI: 10.1097/CCE.0000000000001135 https://journals.lww.com/ccejournal/fulltext/2024/08000/dynamically_normalized_pupillometry_for_detecting.2.aspx